Clinical decision support (CDS) gets most of the attention, but many of AI’s most reliable gains in healthcare come from operations and patient engagement. When integrated with your EHR, LIS, PACS, scheduling, and revenue systems, AI can forecast demand, reduce denials, and personalize outreach—without changing clinicians’ medical decision-making. Here is a practical blueprint for value you can realize now.
Operational intelligence: predict demand and protect capacity
Using historical encounters, referral trends, seasonality, and local events, AI can forecast clinic and ED volumes days to weeks ahead. These signals drive staffing rosters, imaging schedules, and supply ordering to reduce bottlenecks and overtime. Integration matters: ingest HL7 ADT and scheduling feeds, publish forecasts to operations dashboards, and notify managers when thresholds are exceeded.
Revenue cycle: fewer denials, faster cash
Denials are expensive and predictable. AI can score claims for denial risk pre-submission, identify missing documentation, and highlight payer-specific pitfalls. On inbound transactions, classification models route payer responses and prior authorization updates automatically and extract key fields from attachments. The goal is to surface issues early and focus billing experts where their work has the highest financial impact.
Prior authorization and referral triage
Integrate AI to read referral notes and determine likely PA requirements based on payer policy metadata, producing a checklist of missing elements and suggested tasks. This shortens cycle time and reduces back-and-forth. Results can be posted back as work queue items or FHIR Task resources with auditable status changes.
Patient engagement that respects context
AI can tailor reminders and instructions to a patient’s language, reading level, and preferred channel. Examples include pre-visit prep, imaging prep reminders, and lab follow-up nudges. Integrated correctly, messages pull live context from the EHR and push updates back as encounters or communication notes, preserving a complete record of what was sent and when.
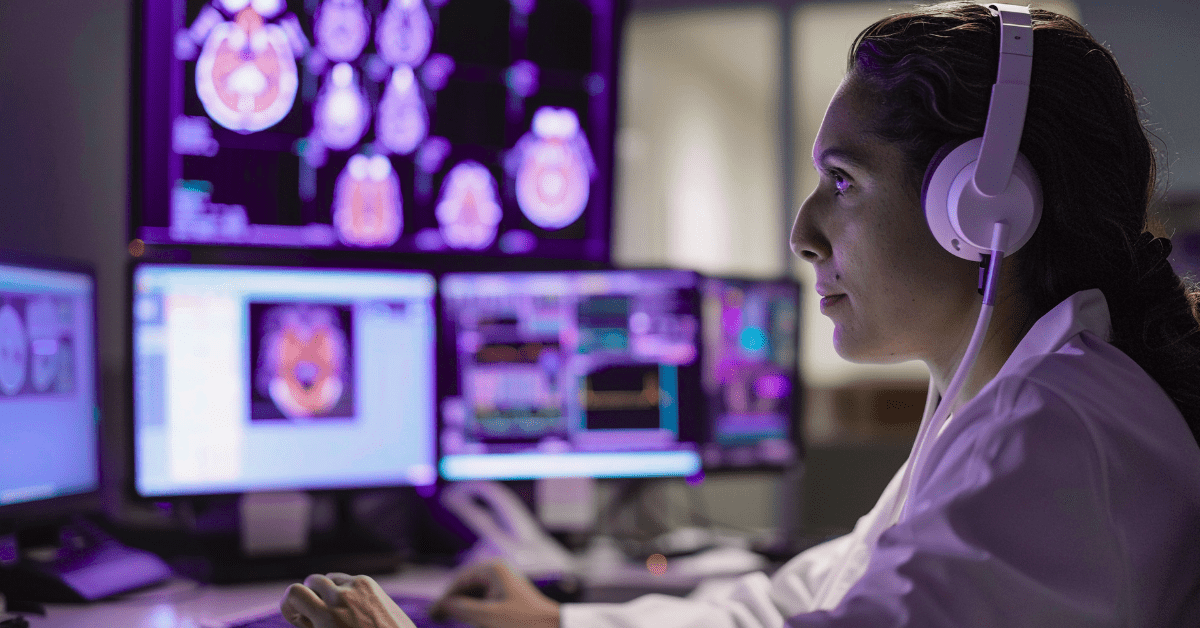
Labs and imaging: workflow acceleration (not diagnosis)
Outside diagnostic claims, AI can streamline operations: normalize external result status codes, predict which accessions may need reflex testing based on ordering patterns, and prioritize worklists using operational metadata (for example, aging STAT orders). Keep clinical interpretation with clinicians; use AI to route the right work to the right place in time.
Integration patterns that keep systems in sync
- HL7 v2 feeds for orders, results, and status changes to drive low-latency triggers.
- FHIR APIs and Subscriptions for structured resource updates and reliable writes.
- Event streaming to decouple AI services from source systems and control retries.
- API gateways with throttling and SLOs to protect clinical and revenue systems.
Guardrails: safety, bias, and compliance
Use minimum-necessary data and PHI-safe prompts. Keep clear audit trails (prompts, inputs, model versions, outcomes). Prefer vendors with BAAs and policies that do not train on your PHI by default. Monitor for drift and run regular bias reviews, especially for models influencing access, scheduling, or financial decisions.
Roadmap to value
- Discovery: choose one high-friction workflow with measurable KPIs (denial rate, no-show rate, overtime hours).
- Pilot: integrate AI under tight guardrails, keep a human-in-the-loop, and measure against baseline.
- Scale: expand to adjacent workflows only after safety and ROI are proven.
- Operate: add monitoring, alerting, and change management so gains persist.
Partner with experts in healthcare interoperability
AI delivers the most impact when it is wired cleanly into your HL7 and FHIR flows, RCM tools, and scheduling systems. Healthcare Integrations builds vendor-agnostic integrations that respect compliance and operational realities. Learn more on our AI Integration Services page, and explore related capabilities in RCM Integration and PACS Integration.